Exogenous Surfactant: A Lifeline for Newborns
The miracle of birth is often accompanied by unforeseen challenges, especially for premature infants. One such challenge is Respiratory Distress Syndrome (RDS), primarily caused by a deficiency of pulmonary surfactant. This is where exogenous surfactant steps in as a critical intervention, quite literally a lifeline for these vulnerable newborns. This article delves into the what, why, and how of exogenous surfactant, its impact on infant health, and the ongoing research shaping its future.
Understanding Respiratory Distress Syndrome (RDS)
RDS, also known as Hyaline Membrane Disease (HMD), primarily affects premature babies whose lungs are not yet fully developed. Surfactant, a complex mixture of lipids and proteins, is produced in the lungs and reduces surface tension, allowing the alveoli (tiny air sacs) to inflate easily and remain open during breathing. Without sufficient surfactant, the alveoli collapse, making it difficult for the infant to breathe. This leads to a cascade of complications, including hypoxemia (low blood oxygen), hypercapnia (high blood carbon dioxide), and potential brain damage.
The Role of Surfactant
Imagine blowing up a balloon. Initially, it requires a lot of effort to inflate it. But once it’s partially inflated, it becomes easier. Surfactant performs a similar function in the lungs. It reduces the surface tension within the alveoli, making it easier to inflate them with each breath. Without surfactant, the baby must exert significantly more effort to breathe, often leading to exhaustion and respiratory failure. Exogenous surfactant aims to mimic this natural process, providing the necessary support for the lungs to function effectively.
What is Exogenous Surfactant?
Exogenous surfactant is a synthetic or animal-derived surfactant administered to infants with RDS to improve lung function. It’s essentially a replacement therapy, providing the missing surfactant that the baby’s lungs are unable to produce adequately. There are several types of exogenous surfactant available, each with its own composition and method of production. These include:
- Animal-derived surfactants: These are extracted from the lungs of animals, typically cows (bovine) or pigs (porcine). They contain a mixture of phospholipids and proteins, closely mimicking the natural surfactant found in human lungs. Examples include Beractant (Survanta), Calfactant (Infasurf), and Poractant alfa (Curosurf).
- Synthetic surfactants: These are manufactured in a laboratory and consist of synthetic phospholipids and, in some cases, synthetic proteins. These are designed to mimic the function of natural surfactant. An example includes Lucinactant (Surfaxin), although it is no longer commercially available in the US.
The choice of surfactant depends on several factors, including availability, cost, and the specific needs of the infant. Studies have shown that both animal-derived and synthetic surfactants are effective in treating RDS, although some studies suggest that animal-derived surfactants may be slightly more effective in reducing mortality and the need for mechanical ventilation.
Administration of Exogenous Surfactant
Exogenous surfactant is typically administered through an endotracheal tube (ETT), a tube inserted into the baby’s trachea (windpipe). The surfactant is instilled directly into the lungs, allowing it to spread and coat the alveoli. The procedure is usually performed in the neonatal intensive care unit (NICU) by trained medical personnel. There are different methods of administration, including:
- Bolus administration: The surfactant is given as a single, large dose.
- Multiple small doses: The surfactant is divided into smaller doses and given over a period of time.
- INSURE (INtubate, SURfactant, Extubate): This involves intubating the baby, administering surfactant, and then quickly extubating (removing the breathing tube) the baby, allowing them to breathe on their own or with less invasive support.
- Less Invasive Surfactant Administration (LISA): This method involves using a thin catheter to administer surfactant directly into the trachea without intubation.
The choice of administration method depends on the baby’s condition and the preferences of the medical team. The goal is to distribute the surfactant evenly throughout the lungs to maximize its effectiveness. The use of exogenous surfactant requires careful monitoring of the infant’s respiratory status, including oxygen saturation, blood gases, and chest X-rays.
Benefits and Risks of Exogenous Surfactant
The benefits of exogenous surfactant therapy are well-established. It can significantly improve lung function, reduce the need for mechanical ventilation, and decrease the risk of mortality in infants with RDS. Specifically, exogenous surfactant contributes to:
- Improved oxygenation
- Reduced lung injury
- Decreased risk of pneumothorax (collapsed lung)
- Shorter hospital stays
However, like any medical intervention, exogenous surfactant therapy is not without risks. Potential complications include:
- Transient hypoxemia (temporary decrease in blood oxygen)
- Bradycardia (slow heart rate)
- Airway obstruction
- Pulmonary hemorrhage (bleeding in the lungs)
- Infection
These risks are relatively rare and are typically outweighed by the benefits of surfactant therapy. Careful monitoring and management can help minimize these complications. The success of exogenous surfactant is undeniable in the landscape of neonatal care.
The Impact on Infant Mortality and Morbidity
The introduction of exogenous surfactant therapy has revolutionized the treatment of RDS and has had a profound impact on infant mortality and morbidity rates. Prior to the availability of surfactant, RDS was a leading cause of death in premature infants. With the widespread use of exogenous surfactant, survival rates for these babies have significantly improved. Furthermore, surfactant therapy has been shown to reduce the long-term complications associated with RDS, such as chronic lung disease (bronchopulmonary dysplasia or BPD). The development of exogenous surfactant represents a major advancement in neonatal medicine, offering hope and improved outcomes for countless premature infants and their families. The advancements in exogenous surfactant administration are also contributing to better outcomes.
Ongoing Research and Future Directions
Research on exogenous surfactant continues to evolve, with ongoing efforts to improve its effectiveness, reduce its risks, and develop new and innovative delivery methods. Some areas of focus include:
- Development of synthetic surfactants with improved efficacy and safety profiles: Researchers are working to create synthetic surfactants that more closely mimic the properties of natural surfactant and are less likely to cause adverse effects.
- Optimization of surfactant administration techniques: Studies are investigating different methods of surfactant administration, such as LISA, to minimize the need for intubation and mechanical ventilation.
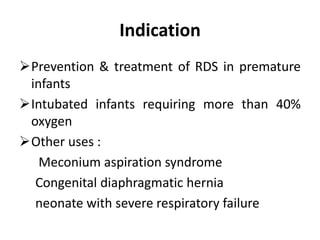
- Investigation of the role of surfactant in other respiratory conditions: Researchers are exploring the potential use of surfactant in the treatment of other respiratory conditions, such as meconium aspiration syndrome and pneumonia.
- Developing personalized surfactant therapy: Tailoring the type and dose of surfactant to the individual needs of each infant.
These ongoing research efforts hold promise for further improving the outcomes of infants with RDS and other respiratory conditions. [See also: Novel Surfactant Delivery Methods] The continuous refinement of exogenous surfactant is a testament to the dedication of researchers and clinicians to improving the lives of vulnerable newborns.
Conclusion
Exogenous surfactant is a life-saving therapy for premature infants with RDS. Its ability to improve lung function, reduce the need for mechanical ventilation, and decrease mortality rates has transformed the landscape of neonatal care. While potential risks exist, the benefits of surfactant therapy far outweigh the risks for most infants. Ongoing research is focused on further improving the effectiveness and safety of surfactant, as well as exploring its potential applications in other respiratory conditions. As we continue to advance our understanding of surfactant and its role in lung function, we can expect to see even greater improvements in the outcomes of infants with RDS in the years to come. The impact of exogenous surfactant on neonatal care cannot be overstated.
